Introduction: The Surprising Link Between Gut and Mind
For decades, anxiety has been primarily understood through the lens of psychology and brain chemistry. Medications and talk therapies have dominated treatment approaches, but recent science reveals a new frontier: the gut. The gut-brain connection is emerging as a powerful axis influencing mood, cognition, and emotional regulation. What once seemed like separate systems are now recognized as intimate partners in health and disease. Anxiety and gut health are not just connected—they may be best friends, intricately communicating through a vast network of nerves, hormones, and microbes. This article dives deep into the microbiome-emotion axis, exploring how nurturing your gut can become a foundational strategy for cultivating mental resilience and transforming anxiety from within.
Understanding the Gut-Brain Axis
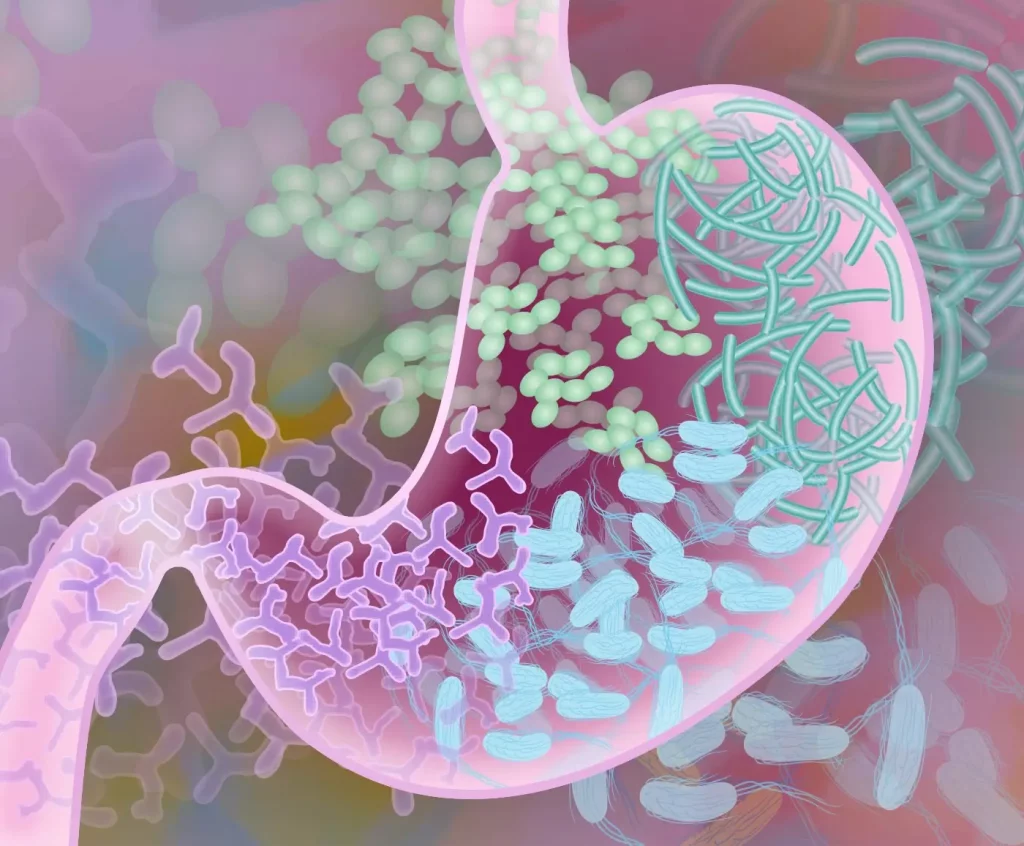
The gut-brain axis is a bidirectional communication system linking the central nervous system (CNS) and the enteric nervous system (ENS)—the “second brain” housed in the digestive tract. These two systems talk via neural pathways (primarily the vagus nerve), immune signaling, and chemical messengers like neurotransmitters and hormones. The gut’s nervous system contains about 100 million neurons, nearly as many as the spinal cord, making it a complex processing center in its own right.
Beyond nerves, the gut hosts trillions of microbes—bacteria, viruses, fungi—that collectively form the microbiome. This ecosystem influences digestion, immune function, and importantly, the production of neuroactive substances like serotonin, dopamine, and gamma-aminobutyric acid (GABA), which regulate mood and anxiety levels. Scientists now understand that changes in the microbiome can profoundly affect mental health, shifting anxiety states through the gut-brain axis.
Microbiome Composition and Anxiety
Research reveals that people with anxiety disorders often exhibit distinct patterns of gut microbiota compared to healthy individuals. Certain beneficial bacteria, such as Lactobacillus and Bifidobacterium species, are found in lower abundance in anxious populations, while potentially harmful bacteria increase. These imbalances, called dysbiosis, can promote inflammation and disrupt neurotransmitter production.
Inflammation caused by gut dysbiosis triggers systemic immune responses that affect brain function, contributing to anxiety and mood disorders. The “leaky gut” phenomenon, where the intestinal lining becomes permeable, allows bacterial toxins to enter the bloodstream, further fueling neuroinflammation and emotional dysregulation.
This understanding shifts anxiety from being solely a brain-based disorder to a systemic condition intertwined with gut health.
Neurotransmitters Produced in the Gut
Approximately 90% of the body’s serotonin—a key mood stabilizer—is produced in the gut, influencing gut motility and emotional regulation. The microbiome also synthesizes GABA, which has calming effects on the nervous system, and dopamine, involved in motivation and reward.
When the microbiome is out of balance, the production and regulation of these neurotransmitters falter, potentially contributing to anxiety symptoms like restlessness, nervousness, and irritability.
Moreover, short-chain fatty acids (SCFAs), produced by fiber-fermenting bacteria, impact brain health by reducing inflammation and supporting the blood-brain barrier’s integrity. SCFAs are critical in maintaining the neuroimmune environment that underlies emotional balance.
Case Studies Linking Gut Health and Anxiety Relief
Emerging clinical studies demonstrate the potential of gut-focused interventions for anxiety reduction. In one trial, participants with generalized anxiety disorder who took probiotic supplements rich in Lactobacillus and Bifidobacterium reported significant decreases in anxiety symptoms over eight weeks compared to placebo groups.
Another study showed that a diet high in fermented foods, prebiotic fiber, and polyphenols improved microbial diversity and reduced social anxiety symptoms. These findings support the idea that modulating the microbiome can be a complementary strategy alongside conventional therapies.
Functional medicine practitioners increasingly use stool analysis to tailor gut-healing protocols that reduce systemic inflammation and improve mental health outcomes.
The Role of Diet in Supporting the Microbiome-Emotion Axis
Nutrition is foundational to nurturing a healthy microbiome and supporting mental well-being. Diets rich in whole, unprocessed foods—vegetables, fruits, legumes, nuts, seeds, and fermented products—feed beneficial bacteria and promote microbial diversity.
Prebiotic fibers like inulin and fructooligosaccharides serve as food for probiotic bacteria, encouraging their growth and metabolic activity. Fermented foods such as yogurt, kimchi, sauerkraut, and kombucha introduce live cultures that enhance gut flora balance.
Conversely, high consumption of processed foods, sugar, and unhealthy fats can damage the microbiome, provoke inflammation, and worsen anxiety symptoms.
Hydration, mindful eating practices, and avoiding excessive antibiotics or unnecessary medications are also key to maintaining gut health.
Stress, Anxiety, and the Gut: A Vicious Cycle
Stress and anxiety themselves can disrupt gut function. The hypothalamic-pituitary-adrenal (HPA) axis, activated during stress, releases cortisol and other hormones that alter gut motility, increase intestinal permeability, and reduce beneficial bacteria populations.
This creates a feedback loop: anxiety disrupts the gut, and gut imbalance exacerbates anxiety. Breaking this cycle requires simultaneous attention to both mind and gut, using techniques that calm the nervous system and repair microbial health.
Mind-body interventions like mindfulness meditation, yoga, and breathwork help regulate the HPA axis, improving gut symptoms linked to stress.
Emerging Therapies Targeting the Microbiome for Anxiety
Probiotics, often called “psychobiotics” when targeted for mental health, are showing promise in clinical trials. They work by restoring microbial balance and enhancing production of neuroactive compounds. However, the effects are strain-specific, highlighting the importance of personalized approaches.
Fecal microbiota transplantation (FMT), though still experimental for mental health, offers another avenue to reset the microbiome in severe cases.
Nutritional psychiatry—a field integrating diet, microbiome, and mental health—advocates for dietary interventions as adjunctive treatments for anxiety and depression.
Prebiotics and postbiotics, supplements that feed beneficial bacteria or provide bacterial metabolites, also represent cutting-edge options under study.
Gut Healing Practices Beyond Diet
In addition to nutrition, several lifestyle factors support a healthy gut-brain connection:
- Regular physical activity promotes microbial diversity and reduces systemic inflammation
- Quality sleep maintains circadian rhythms essential for gut and brain function
- Avoiding environmental toxins such as pesticides and excessive alcohol protects microbiome integrity
- Social connection and emotional support positively influence gut health through stress reduction
- Mindful breathing stimulates the vagus nerve, enhancing parasympathetic tone and digestive regulation
Challenges and Considerations in Gut-Anxiety Research
While promising, the field faces challenges. Individual microbiomes vary widely, complicating universal recommendations. Many studies are small or preliminary, necessitating further research to clarify mechanisms and optimize treatments.
Additionally, anxiety is multifactorial, with psychological, social, and genetic components that interplay with gut health. Integrative approaches combining conventional psychiatry with gut-focused strategies are most effective.
Ethical considerations include avoiding oversimplification of mental health issues and recognizing that gut healing is complementary, not a replacement for professional mental health care.
The Future of Mental Health: Integrative Gut-Brain Care
The growing awareness of the microbiome-emotion axis signals a paradigm shift in mental health care. Future treatments will likely integrate microbiome modulation with psychotherapy, pharmacology, and lifestyle interventions.
Personalized microbiome profiling and precision nutrition could tailor anxiety treatments to individual biological needs. Digital health tools may track gut and mood biomarkers to optimize interventions in real time.
This holistic vision honors the complexity of human health, recognizing that mental resilience springs from a harmonious body-mind ecosystem.
Practical Tips to Nurture Your Gut and Anxiety Resilience
- Incorporate fermented foods and prebiotic fibers daily
- Minimize processed foods and added sugars
- Manage stress through mindfulness, yoga, or breathwork
- Prioritize consistent, restorative sleep
- Stay physically active and hydrated
- Seek professional guidance for persistent anxiety or gut issues
- Consider probiotic supplementation after consulting a healthcare provider
Conclusion: Embracing the Friendship Between Gut and Anxiety
Anxiety and gut health are deeply intertwined partners in our emotional landscape. Understanding the microbiome-emotion axis transforms anxiety treatment from a narrow brain-centric model into a rich, embodied approach.
Healing the gut nurtures the mind, bolsters resilience, and opens pathways to lasting emotional well-being. As science uncovers the secrets of this relationship, we are invited to embrace a new perspective: that caring for our digestive ecosystem is an essential act of self-love and mental health.
By honoring this friendship within, we can unlock the transformative power of gut healing for anxiety relief and vibrant mental resilience.







































