Introduction: Why Gut Health is More Than Digestion
In recent years, the phrase “gut feeling” has gained a whole new layer of scientific credibility. No longer just a metaphor for intuition, the gut—specifically the gut microbiome—has emerged as a powerful regulator of brain function and emotional well-being. A growing body of research is revealing an intricate, bi-directional communication system between the gastrointestinal tract and the brain, known as the gut-brain axis. This system is reshaping our understanding of mental health, highlighting how imbalances in gut bacteria can contribute to anxiety, depression, and cognitive dysfunction. As researchers dive deeper into the complexities of the gut microbiome, they’re uncovering groundbreaking strategies for emotional healing that start from the inside out—beginning in the belly.
Understanding the Gut-Brain Axis
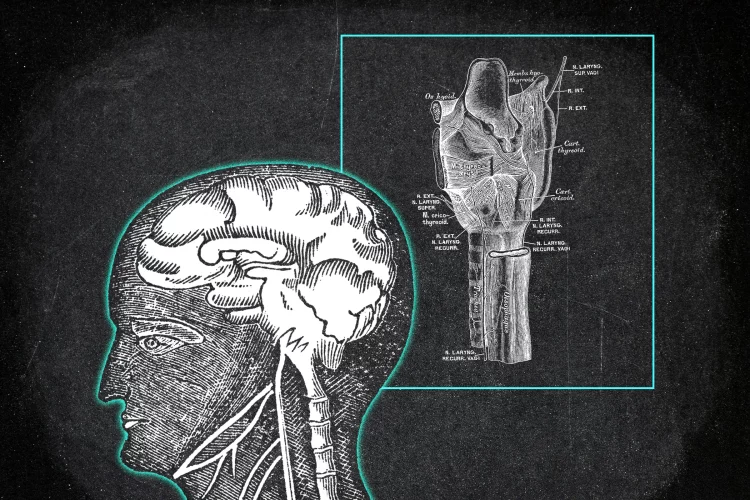
The gut-brain axis is a complex network that connects the enteric nervous system (ENS) of the gastrointestinal tract with the central nervous system (CNS). This system communicates through a variety of pathways—neural (vagus nerve), endocrine (hormones), immune (cytokines), and metabolic (short-chain fatty acids). Far from being just a “food processing” unit, the gut is now often referred to as the “second brain.” It houses over 100 million neurons and produces nearly 95% of the body’s serotonin, a key neurotransmitter involved in mood regulation. The vagus nerve plays a critical role in this relationship, acting as a communication superhighway that transmits information from the gut to the brain and vice versa. Disruptions in this communication channel have been linked to a range of psychological disorders, including depression and anxiety.
The Microbiome: Your Inner Ecosystem
At the heart of the gut-brain axis lies the microbiome, the trillions of bacteria, viruses, and fungi residing in the gastrointestinal tract. These microorganisms perform essential tasks: aiding in digestion, producing vitamins, synthesizing neurotransmitters, and modulating the immune system. A healthy microbiome fosters a balanced emotional state, while dysbiosis—a state of microbial imbalance—has been associated with numerous mood disorders. Several studies have shown that individuals with major depressive disorder often have a distinct microbial signature compared to healthy individuals. In mouse models, transferring gut bacteria from depressed humans to germ-free mice has induced depression-like symptoms in the animals, further validating the gut’s influence on mental health.
The Science Linking Gut Health and Mental Disorders
Multiple research avenues are converging on the idea that gut microbiota influence mood and cognitive function. One of the most cited studies in this field, published in Nature Microbiology, found that specific bacterial genera, such as Coprococcus and Faecalibacterium, were consistently depleted in people suffering from depression. These bacteria are known to produce short-chain fatty acids (SCFAs) like butyrate, which have anti-inflammatory properties and maintain the integrity of the blood-brain barrier. Inflammation, both systemic and neuro-inflammation, is increasingly recognized as a contributing factor to mood disorders. Gut-derived inflammatory cytokines can reach the brain and disrupt neurotransmitter metabolism, neuronal signaling, and neuroplasticity, creating fertile ground for anxiety and depression.
Psychobiotics: Bacteria That Boost Mood
Psychobiotics is an emerging class of probiotics that are specifically targeted to improve mental health. These beneficial bacteria, such as Lactobacillus rhamnosus, Bifidobacterium longum, and Lactobacillus helveticus, have been shown to modulate the stress response, reduce inflammation, and enhance the production of mood-regulating neurotransmitters. In a randomized controlled trial, participants who consumed a psychobiotic formulation reported lower levels of cortisol and fewer symptoms of anxiety and depression compared to those taking a placebo. Another study demonstrated that Bifidobacterium longum NCC3001 significantly reduced depression scores in patients with irritable bowel syndrome, highlighting the interconnectedness of gut health and emotional well-being.
Dietary Interventions to Improve Gut and Mental Health
What you eat can significantly influence your gut microbiota and, by extension, your mental state. A Mediterranean-style diet rich in fiber, fruits, vegetables, legumes, and whole grains has been associated with reduced risk of depression. Fermented foods like kefir, yogurt, kimchi, and sauerkraut provide a natural source of probiotics, while prebiotics—non-digestible fibers found in foods like garlic, onions, leeks, and bananas—serve as fuel for beneficial bacteria. Omega-3 fatty acids found in fatty fish like salmon and sardines also support a healthy microbiome and reduce inflammation. Limiting sugar, processed foods, and artificial sweeteners is crucial, as these can disrupt the microbial balance and increase gut permeability, often referred to as “leaky gut,” which is implicated in systemic inflammation and mental health issues.
Holistic Gut-Balancing Protocols
Balancing the gut for better mental health goes beyond just dietary changes. A comprehensive approach involves managing stress, prioritizing sleep, incorporating regular physical activity, and avoiding unnecessary antibiotics. Mindfulness-based stress reduction (MBSR), yoga, and deep-breathing exercises have all been shown to positively affect the gut microbiome and the gut-brain axis. Sleep deprivation alters the composition of the gut microbiota, and regular exercise fosters microbial diversity. Additionally, gut-healing supplements like L-glutamine, zinc carnosine, and collagen peptides can help restore intestinal lining integrity, further supporting mental clarity and emotional balance.

Case Studies and Real-Life Success
Consider Sarah, a 34-year-old woman who had struggled with anxiety and mood swings for over a decade. Conventional treatment with SSRIs offered limited relief and came with unpleasant side effects. Upon working with a functional medicine practitioner, she underwent a comprehensive stool analysis that revealed dysbiosis and a leaky gut. Through a targeted protocol involving a low-inflammatory diet, high-quality probiotics, stress management, and gut-healing nutrients, she reported significant improvements in her emotional stability and overall quality of life within three months. Similar anecdotal accounts are becoming increasingly common, supported by clinical studies that validate the profound impact of gut-focused interventions on psychological health.
Challenges and Limitations in Current Research
Despite the promising data, the field is not without its limitations. Much of the current research is based on animal models or small-scale human studies, making it difficult to generalize findings. Microbiome composition can vary widely among individuals, influenced by genetics, geography, diet, and lifestyle, which complicates the creation of universal treatment protocols. Additionally, we are only beginning to understand the complex interactions between microbial species and their metabolites. There’s also a lack of standardized diagnostic tools to assess gut-brain dysfunction, making it challenging for practitioners to measure and monitor progress accurately. Nonetheless, the trajectory of research is encouraging, and larger, more rigorous studies are currently underway.
Future Directions: Personalized Psychobiotics and AI-Powered Gut Analysis
Looking ahead, the future of gut-brain medicine lies in personalization. With advancements in genomics, metabolomics, and AI, we are moving toward customized probiotic formulations tailored to an individual’s unique microbiome profile. Startups are already offering at-home stool testing kits that analyze microbial composition and provide personalized dietary recommendations. AI algorithms are being trained to predict mood disorders based on microbial markers, which could revolutionize early diagnosis and intervention strategies. Furthermore, combining psychobiotics with conventional psychiatric treatments could offer a synergistic approach that maximizes therapeutic outcomes with fewer side effects.
Conclusion: Healing the Mind Starts in the Gut
The evidence is clear: gut health and mental health are inextricably linked. Far from being an isolated system, the gut communicates continuously with the brain, influencing mood, behavior, and cognitive function. As science peels back the layers of this intricate relationship, it becomes increasingly evident that true emotional healing must take the gut into account. Whether through dietary changes, targeted probiotics, or holistic lifestyle interventions, nurturing your inner ecosystem offers a transformative pathway to mental wellness. In the future, managing depression and anxiety may involve not just therapy or medication, but a visit to the nutritionist or even a personalized gut-microbiome clinic. In this new paradigm, healing your mind may begin with healing your gut—and that’s a change we can all digest.